At Community Catalyst we are often asked for lessons or insights into the Community Health Needs Assessments that non-profit hospitals have been generating. In fact, we are in regular communication with several groups around the country who are monitoring Community Health Needs Assessments (CHNAs) in their communities. We asked one of our partners, Georgia Watch, to share some highlights from their review of several first round CHNAs and implementation strategies produced in Georgia during 2012-2013. Their research offers valuable insights into the processes hospitals used and the opportunities for advocates and community-based organizations to engage with their hospitals as the next round of CHNAs are conducted in 2015-2016. For more resources and tools to support this work, please visit our website.
-Michele Craig, Hospital Accountability Project
Georgia Watch is a statewide consumer advocacy organization based in Atlanta, Georgia. The Nonprofit Hospital Community health Needs Assessments in Georgia report reflects our recent efforts to review the initial CHNAs and available implementation strategies for 38 non-profit hospital facilities throughout Georgia. Our goal was to understand whether hospitals were complying with the community benefit requirements established in the Affordable Care Act (ACA). The ACA included important provisions around hospital community benefit and mandates that all 501(c)(3) non-profit hospitals conduct a CHNA and write a corresponding implementation strategy every three years. The ACA requires that hospitals seek input from community members and public health when conducting CHNAs.
As part of our research for the report, we developed evaluation tools to assess hospital compliance with five major components of the new ACA requirements: 1) defining community; 2) collecting secondary data on community health; 3) gathering community input and primary data; 4) prioritizing community health needs; and 5) implementing strategies to address identified community health needs. We also conducted interviews with hospital leadership and surveyed those community members who provided input into their local hospital’s CHNA to gain a deeper understanding of the hospital processes used in 2012-2013.
The CHNAs varied tremendously. Some were very robust with a 200+ page length, while others were less than 10 pages and lacking in detail and transparency. From this review, we identified key takeaways and recommendations for moving forward.
Defining Community
- When defining community, only 28 (74 percent) of the hospitals clearly articulated how they defined their communities, despite the IRS requirement that they do so.
- Twenty-five hospitals (66 percent) used internal hospital utilization data, such as admissions and discharges, to either define their communities or assess the health needs of their communities in their CHNAs.
Community Input
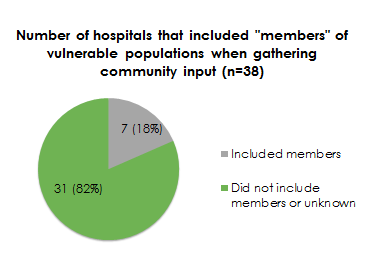
- All 38 hospitals gathered input from their community through surveys, interviews, focus groups or community meetings, but only seven (18 percent) explicitly and intentionally gathered input from members of vulnerable populations.
- Only 12 hospitals incorporated community members into their CHNA project leadership teams.
- Thirty-one hospitals (82 percent) stated that they collected input from county or regional health departments in their service areas.
Secondary Data Collected
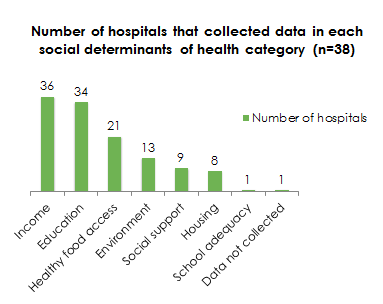
- Hospitals most frequently gathered and reported data on the following social determinants of health: education level, income, and healthy food access.
- Only thirteen hospitals (34 percent) collected data on environmental health indicators, including public safety, transportation, parks, pollution, and water quality.
Prioritizing Needs
- Seven of the 38 hospital CHNAs (18%) reviewed failed to describe how they prioritized community needs with any amount of detail, despite the IRS requirement that they do so.
- Only eleven of the 31 hospitals that articulated how they prioritized community health needs clearly incorporated community representatives into their needs prioritization process.
- No hospitals prioritized health needs related to physical environment, such as improving housing or building parks.
- The most common community health needs prioritized by hospitals were those related to chronic diseases, such as heart disease, cancer, obesity, and diabetes.
Implementation Strategies
- Only 16 of the 29 hospital implementation strategies (55 percent) reviewed included an anticipated impact or method of measuring the impact of their programs.
Recommendations
- When defining community, hospitals should identify and focus on vulnerable populations, even if they are not the hospitals’ traditional service-seeking patients, and they should examine their emergency room utilization data to better understand the needs of the vulnerable community members they serve.
- Hospitals should gather input from members of vulnerable populations when assessing community health needs and incorporate community members into their prioritization and implementation processes.
- Hospitals should also engage in partnerships with local health departments and community-based organizations, as collaboration and coordination are keys to improving community health.
In order to improve transparency and inclusion in the CHNA process, it is critically important for individuals outside of hospital administration to understand what is required of hospitals in conducting CHNAs. Community groups and advocacy organizations must remain vigilant in order to keep non-profit hospitals working cooperatively with public health departments and community-based organizations to improve population health.
We hope that our report provides community members with the knowledge they need to evaluate the adequacy of CHNAs from nonprofit hospitals within their communities, engage with hospitals in the CHNA process, and encourage their local hospitals to develop impactful community benefit programs.
If interested, please also read our recently released companion report that traces the evolution of the IRS regulations governing the CHNA process, from the initial IRS Notice in 2011 to the final regulations published at the end of 2014.
The project described in this post was funded solely by the Healthcare Georgia Foundation. Created in 1999 as an independent private foundation, the Healthcare Georgia Foundation's mission is to advance the health of all Georgians and to expand access to affordable, quality healthcare for underserved individuals and communities.
– Beth Stephens, J.D., Health Access Program Director, Georgia Watch
