This is the second blog in a series to highlight the dangers of the repealing the Affordable Care Act. Multiple times a week, Community Catalyst will highlight a different constituency to draw attention to the benefits the ACA has afforded them and to outline what a loss of coverage would mean.
In 2015, Belhaven, North Carolina Mayor Adam O’Neal and supporters from 11 other states set out on foot for their second 300-plus mile trek from his rural town to our nation’s capital to draw attention to an important issue: rural communities in danger of their hospitals closing.
The walk idea was sparked when O’Neal’s local hospital, Vidant Pungo, closed its doors in July 2014. For many in that small town, not only were those hospital jobs lost, but the nearest hospital is now 30 miles away. Sadly, this is a scenario being replicated all across America. A major source of rural hospitals’ financial stress can be traced to their state decisions to turn down federal funding to cover more people through Medicaid. With some Republicans in Congress and the incoming Trump Administration bent on repealing the Affordable Care Act (ACA) with no plan to replace it, we seem to be moving further from finding a solution to this crisis.
For the 50 million Americans living in rural parts of the country, accessing health care has often meant facing a variety of barriers: difficulty making an appointment with a provider or specialist, traveling long distances to the nearest hospital, and a high rate of local hospitals closing their doors. People living in rural areas will have even more to lose if the incoming administration dismantles the gains we've made under the ACA.
Figure A. Rural Counties Across the U.S.
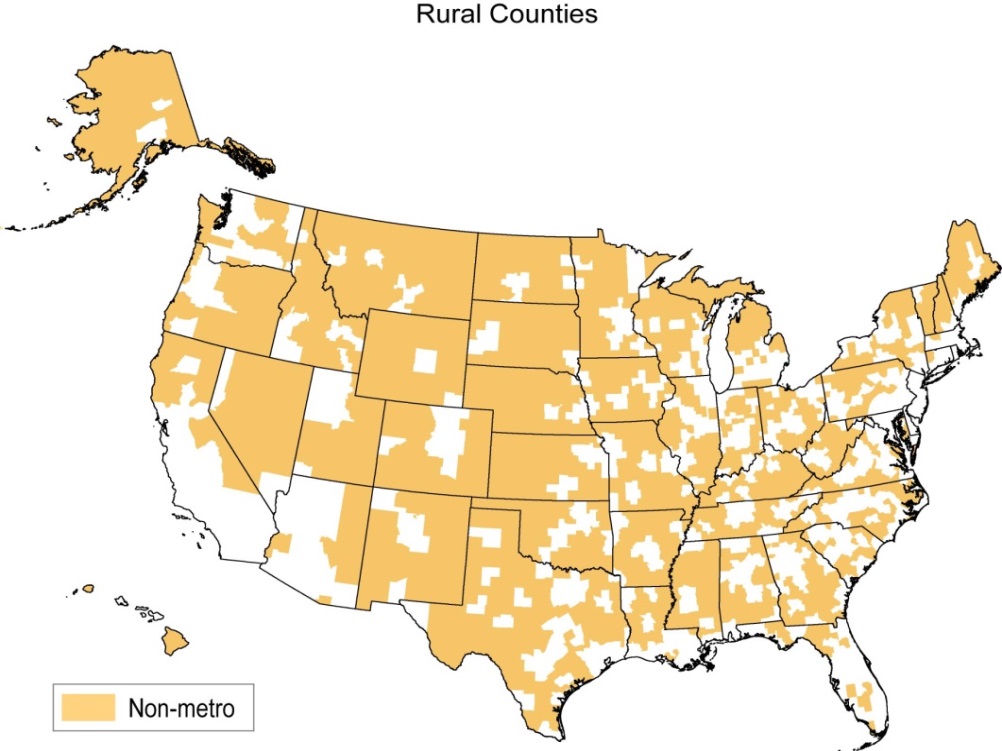
In the past six years, while millions of Americans have benefited from the ACA, Americans living in rural areas have made more progress under the ACA than the general population. People living in rural communities saw a 7.2 percentage point increase in coverage from 2013 to 2015, compared with a 6.3 percentage point increase for urban individuals. Of the nearly 2 million rural customers who bought health coverage through the ACA Marketplace in 2016, about 9 out of 10 rely on tax credits to make their coverage affordable. Also, because of the ACA, the share of rural Americans who cannot afford necessary care decreased by six percentage points. In real terms this means that families are able to have coverage regardless of their health status and are able to take advantage of financial assistance to make it possible.
But now these much-needed health care gains for rural communities are under threat. Congressional leaders and the incoming administration have indicated the first item on their agenda is repeal of the ACA without a replacement plan (including a repeal of Medicaid expansion). Rural Americans’ health coverage and livelihoods could be hit especially hard.
In addition to historical barriers to care, rural America’s struggles with health care are rooted in policy decisions that have left them worse off. For example, rural individuals are concentrated in states that have resisted reforms available to them under the ACA, like Medicaid expansion. These state decisions have had significant implications: more than a million rural individuals fall into the Medicaid coverage gap and many hospitals in rural areas are unable to draw in the benefits of a more insured patient mix. This is a large reason why more than 70 rural hospitals – most located in non-expansion states – have shut down since 2010. Many more hospitals are at-risk of closing because of financial pressure, in which Medicaid expansion would provide a lifeline. Hospitals are important employers and contributors to the local economy, so these hospital closures are happening to rural communities that can least afford to lose these economic benefits. Our rural communities know all too well the struggles of keeping their communities healthy and safe. Any reforms undertaken on a large national scale should improve health care, not put it in a state of uncertainty (Figure B).
Figure B. Why the ACA is A Critical Lifeline for Rural Communities
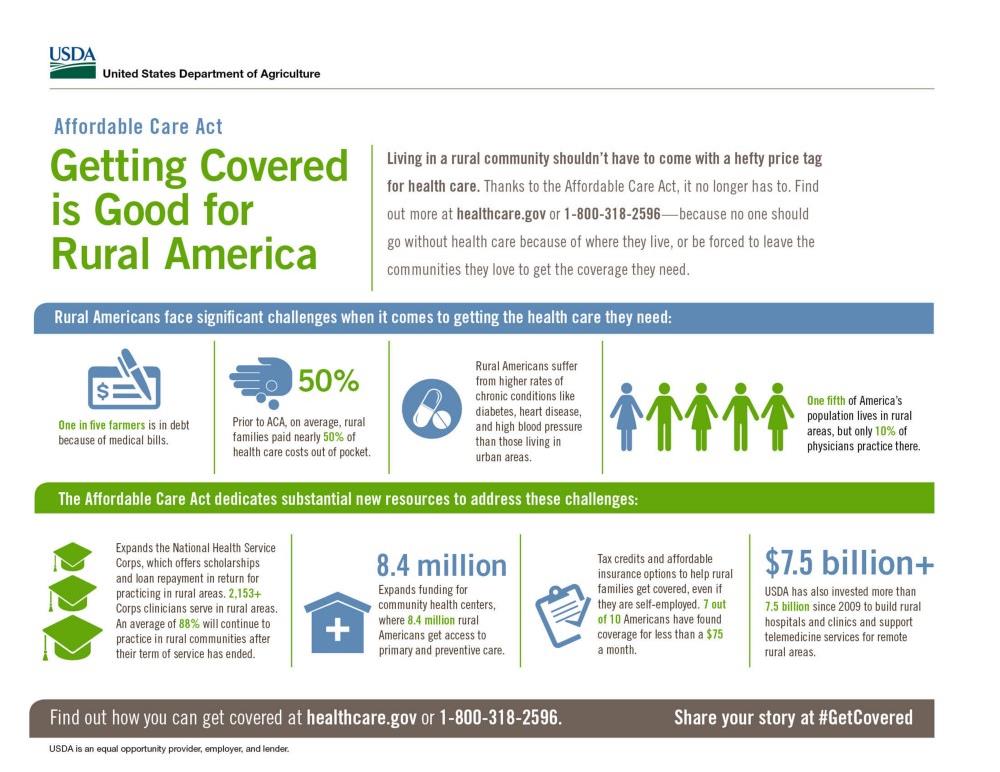
Repealing the ACA without an adequate replacement would shut off any hope of saving these vulnerable communities from additional hospital closures. ACA repeal would also deny a pathway for individuals to gain affordable coverage and endanger gains made in rural communities in states that have embraced the health law.
One state with a lot at stake is Kentucky, which closed the coverage gap and set up its own state-based exchange under the ACA. Because of these decisions, the state’s uninsured rate dropped from 20 percent in 2013 to only 7.5 percent in 2015 – one of the biggest successes in the nation. Rural areas of Kentucky, which have been hard hit by poverty and poor health, disproportionately benefit from these gains in coverage. Ending the health law could be detrimental to in places with a high share of rural communities like Kentucky and Louisiana as well – which also closed their coverage gap in 2016 – where many have been able to obtain health insurance for the first time and use important preventive services that are shown to improve health and cut health costs over the long-term.
Communities are only as healthy as the people that comprise them. When people are healthy, they are able to raise thriving families and contribute to their local economies. This could not be truer in rural America, where the communities here would be in some of the greatest danger if the ACA is repealed without an appropriate replacement plan that protects and expands on the coverage gains of the last six years.
