Last week, Community Catalyst submitted comments to HHS about the Basic Health Program (BHP) option in the Affordable Care Act (ACA.) While there are many reasons to be enthusiastic about BHP, its potential to dramatically lower health care costs for some of the most vulnerable members of our society is by far the most compelling.
The Heart of the Matter Nothing illustrates the benefits of BHP more clearly than this chart from a report by the Urban Institute. It shows health care costs for low-income adults, with and without BHP:
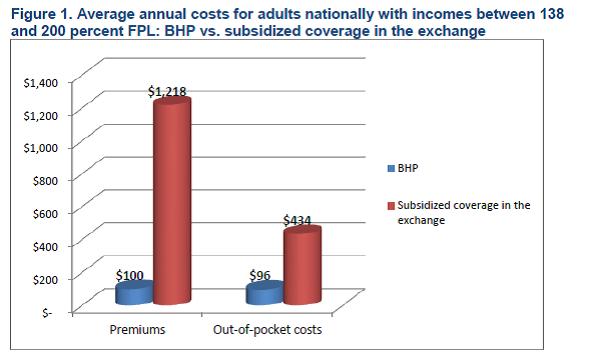
If you’re earning $15,000 a year, $1,500 can make the difference between being able to afford the coverage that you need, and simply going without. The Urban Institute confirms this: they find that if all states took up the Basic Health Plan, coverage rates would increase by 600,000 additional people.
And the benefits of lower health care costs under BHP extend beyond health. An annual survey of New York City residents confirms what those of us who work with this population already know: those earning less than 200 percent Federal Poverty Level (FPL) are just barely able to make ends meet. Forty percent had credit card debt, more than a quarter had unpaid medical bills, and more than a quarter fell behind in rent or mortgage in the last year. For families at this income level, $1,500 can relieve significant financial hardship.
The Basics of the Basic Health Plan BHP is an option in the ACA that gives states the opportunity to provide alternative coverage to two groups of people who would otherwise get coverage through the Exchange:
- • Adults earning just above Medicaid eligibility level but less than 200 percent FPL (about $15,000-$22,000 annually for an individual)
- • Legal immigrants earning under the Medicaid eligibility level (less than $15,000 for an individual), but who do not qualify for Medicaid because of their immigration status
What’s the Catch? The most common concern about BHP is that it will shrink the pool of covered lives in the Exchange, lessening its negotiating leverage with insurers. While we’re interested in pursuing policy options to mitigate any adverse impact on the Exchange (see our comments for more details), we’re not convinced this threat is as significant as it’s been made out to be.
First, it is not clear to what extent states plan to aggressively use the negotiating leverage they have. According to a report by the Kaiser Family Foundation, of the 12 states with established exchanges only five explicitly empowered their Exchanges to act as active purchasers. Many of the remaining states seem reluctant to even establish an Exchange, let alone use it aggressively. And the Urban Report shows that BHP would decrease the number of total enrollees in the Exchange by 16 percent on average. In most states, this is probably not enough to significantly impact Exchange leverage.
Second, most people in the Exchange will not be impacted by a rise in premiums. Over 80 percent of people in the Exchange are receiving premium tax credits, so what they pay towards their premiums is based on a fixed percentage of their income. If the Exchange lowers premiums, the benefit will flow primarily to the federal government in the form of smaller tax credit liabilities.
Only those who don’t qualify for tax credits – primarily people earning above 400 percent FPL – face the full premium. To secure affordable premiums for this population, states can supplement Exchange negotiating leverage with active rate review and regulation of insurance markets both inside and outside the Exchange
At the end of the day, the ACA is about putting health care coverage within the reach of everyone. By lowering health care costs dramatically for the most vulnerable among us, BHP is an essential tool in helping us realize that promise.
--Katherine Howitt, Senior Policy Analyst
