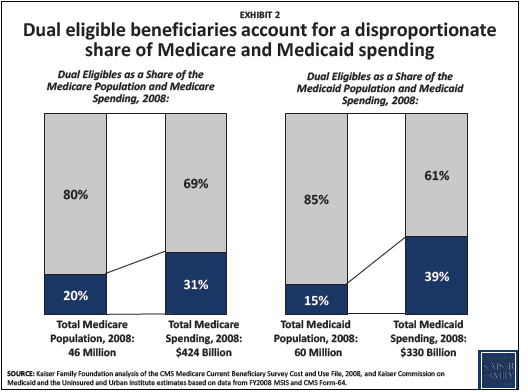
Recently, the Kaiser Family Foundation released helpful new data on the role Medicare and Medicaidprograms play for dually eligible beneficiaries. As a group, these 9 million low-income seniors and people with disabilities tend to have higher rates of chronic disease and make greater use of hospitals, emergency rooms and nursing facilities. As a result, they make up a disproportionate share of spending in in both programs.
 As the pressure to curb health care costs increases, states are moving full steam ahead with a new set of CMS-sponsored initiatives aimed at integrating care for dual eligibles. In fact, with its submission to CMS last week, Ohio is the second state to make a formal proposal for a demonstration project (Massachusetts was the first). While the goals of the overall program are laudable – better care at lower cost – consumer advocates must be aware of the risks and work to make sure the new programs maintain or improve beneficiaries’ access to high-quality, comprehensive care and services.
As the pressure to curb health care costs increases, states are moving full steam ahead with a new set of CMS-sponsored initiatives aimed at integrating care for dual eligibles. In fact, with its submission to CMS last week, Ohio is the second state to make a formal proposal for a demonstration project (Massachusetts was the first). While the goals of the overall program are laudable – better care at lower cost – consumer advocates must be aware of the risks and work to make sure the new programs maintain or improve beneficiaries’ access to high-quality, comprehensive care and services.
Community Catalyst has written an issue briefaimed at helping advocates shape the design and implementation of these new programs. The brief focuses on ten priorities:
- Enrollment
- Provider Networks
- Long-Term Services and Supports
- Coordination
- Benefits
- Consumer Engagement
- Beneficiary Protections
- Financing and Payment
- Quality Measurements
- Cultural Competency
With consumer advocacy on these priority areas, we believe there is a better chance of making real improvements in the health and well-being of high-risk seniors and people with disabilities. At the same time, if done well, these programs may lead to savings that can curb the growth in state and federal health care spending, thereby avoiding harmful cuts to these critical programs. The bottom line? Duals demonstration projects will only achieve their promise if advocates are meaningfully involved, voice their concerns and propose real solutions that work for real people.
-- Leena Sharma, State Advocacy Manager, Integrated Care Advocacy Project
