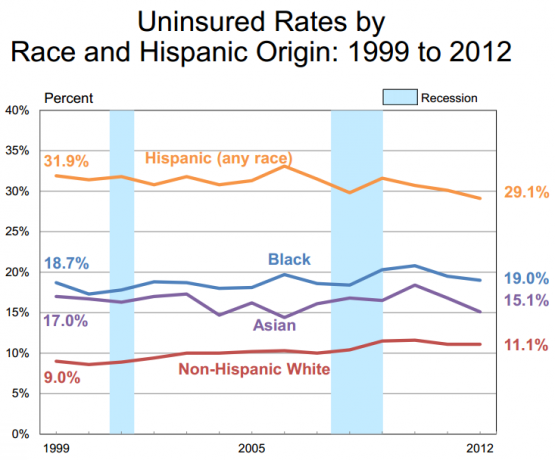
With open enrollment in full swing, consumer health advocates are ramping up their outreach to diverse populations that continue to have disproportionately high rates of uninsurance.
Latinos in particular are more likely to be uninsured, with one in three Latinos lacking coverage nationally. While some states have made great progress in lowering the uninsured rate—states that closed the coverage gap have seen the uninsurance rate among Latinos drop from 36 percent to 23 percent— there is still a lot more work to do to ensure all Latinos can gain access to coverage.
According to recent research, while most uninsured Latinos recognize the value of having health insurance and are interested in seeking health insurance options, 7.6 million o f an estimated 10.2 million of uninsured Latinos who are eligible for Medicaid or financial help to pay for coverage continue to face barriers to enrolling in coverage:
- Lack of Awareness: According to a national poll conducted by the Robert Wood Johnson Foundation (RWJF), 81 percent of participants indicated that they do not know enough about the ACA, 78 percent do not know that the ACA provides financial help, and 66 percent do not know free, in-person assistance is available to help people apply for coverage. According to the same RWJF poll, when asked why they do not have insurance, 36 percent of respondents said they cannot afford insurance or they would not qualify. There is lack of awareness among Latinos about the availability of advanced premium tax credits (APTCs) for legal immigrants even if their income is below 100 percent Federal Poverty Level (FPL) and even if they are not eligible for Medicaid or CHIP under the five year bar.
- Health literacy: Latinos are less likely to understand basic health insurance concepts than white, non-Hispanics. Additionally, some members of the Latino community view health insurance as transactional – something they should pay for as they go.
- Immigration status: Mixed status families (i.e. families or households comprised of undocumented immigrants and United States residents) fear their undocumented relatives will be deported if they apply for insurance coverage and provide information about their household to the Marketplaces.
- Language: There is limited access to accurate Spanish-language materials about the enrollment process. Additionally, CuidadoDeSalud.gov (the Spanish version of healthcare.gov) did not launch until December last year, which limited access to information about open enrollment for native Spanish Speakers.
While there are significant barriers to address in outreach to Latino communities, advocates around the country successfully employed essential strategies to reach uninsured Latinos and help them gain access to health care. (Learn more about these strategies and the outcomes they’ve produced by following the links below.):
- Increasing health literacy and awareness through radio and television: The Colorado Consumer Health Initiative’s Latino Media Project in partnership with Adelante con la Salud (Latino Health Care Engagement Project) worked together to successfully educate Latinos in Colorado about the benefits of the ACA. With the help from Health Care for All Massachusetts (HCFA), they collected success stories about clients who gained coverage, both through expanded access to Medicaid and through financial help. In addition, educational messages about how Latinos benefit from the ACA were also disseminated through radio and television channels in both English and Spanish.
- Engaging the faith-based community through education and enrollment events: UHCAN Ohio built strong relationships with community and faith based organizations by educating organizations about the ACA and partnering with them in Marketplace outreach, enrollment, and follow-up efforts recruiting some in Medicaid and marketplace outreach, enrollment, and follow-up efforts. Some community and faith groups then hosted enrollment events and others became certified application counselors. With the relationships they’ve already had with the local community, they partnered with church leaders in Latino communities to help them serve as health care resources for their congregations.
- Training the trainer: The Oregon Latino Health Coalition hosted a conference to train 200 community health workers on how to assist Latino families with enrollment. In Florida, groups like the Epilepsy Foundation of Florida trained Navigators and teaming up with hospitals to reach Latinos.
- In-person assistance: A personal touch is crucial during successful enrollment. Recent message research has shown that many members of the Latino population value a human interaction to answer questions and allay fears surrounding the enrollment process.
- Using trusted messengers: the Latino community almost unanimously point to their social circle as their first and most trusted source of information
While it was difficult for advocates to reach and enroll some populations, especially the Latino population, the examples above can provide a roadmap to effectively working with the Latino population. For the second open enrollment period, advocates will need to continue focusing on outreach efforts for the uninsured Latino population, and use the information gained through polling and message research to pivot their efforts toward improving health literacy and adding a personal touch to enrollment assistance.
