Photo credit: bigstockphoto.com
An Important Step on the Road to Equity and Universal Coverage
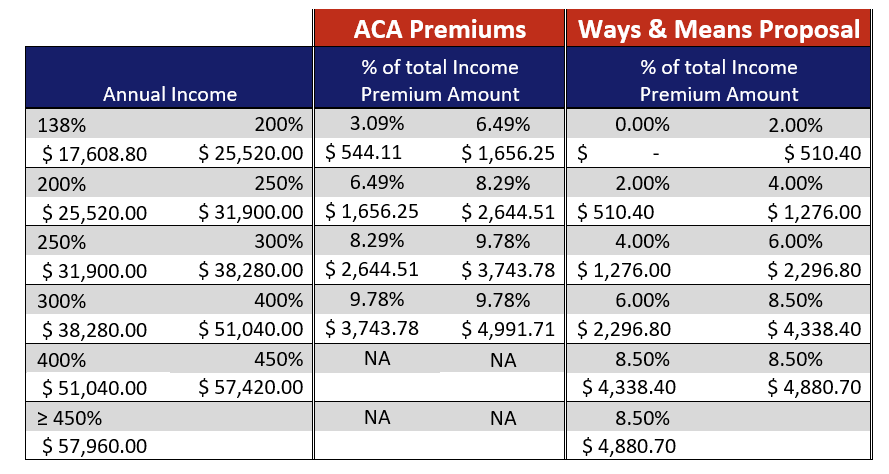
Last night, the House Ways and Means Committee released language outlining their approach to improving subsidies, aligning themselves with the Biden COVID Relief package framework. This is a most welcome development, setting the table for more affordable coverage for millions. Since its passage, the Affordable Care Act has made health care more accessible and affordable for tens of millions of people. But the ACA suffers from a number of shortcomings. High on that list is inadequate premium assistance for millions of low- and moderate-income people. Since the ACA “went live” it has become clear that high premiums still remain a barrier to coverage for tens of millions of people, especially those with low and moderate incomes.
Evidence that more needs to be done to make premiums affordable comes from both the uninsured — who cite affordability as the biggest barrier to coverage — and from those who get their care on the Marketplace, with over 45% of subsidized enrollees in all income brackets reporting some or great difficulty affording premiums.
While low-income people — income below 200% of the Federal Poverty Level (FPL) — have seen the biggest coverage gains of any income group, they still have highest uninsured rate, and comprise the largest share of uninsured people. Disproportionately, this group is comprised of people of color who have faced years of discrimination in employment and education and who are therefore more concentrated in low-wage jobs without good benefits.
Getting ACA premium assistance right is one of several steps that can advance us toward greater health care and economic equity and security.[i] Fortunately, President Biden and Congress seem willing to address the issue. In the just-released COVID relief package, House Ways and Means chair Richard Neal has laid out a plan for major improvements in the ACA affordability scale, even doing better than last year’s Affordable Care Enhancement Act
Under current law, a person with income below 150% of the FPL, or $19,140, has to pay 4.14% of their income, or $792 for coverage. This can represent an insurmountable barrier to coverage for these very-low-income households. As noted above, despite gains, most of the remaining uninsured are concentrated at the lower end of the income scale. In addition, we know that low-income people are extremely price sensitive when it comes to purchasing insurance, while evidence from states like Massachusetts and New York that have very low premiums (along with no deductible and low cost sharing) for people with incomes below 200% FPL have a strong enrollment track record.
Raising premium subsidies at the bottom of the income scale will also help address income inequality. Incomes in the lowest quintile have stagnated for the past 40 years while the cost of many core necessities, such as housing, food and of course health care, have risen faster than the CPI overall.
Under the revisions proposed by Ways and Means, premiums would be eliminated for those below 150% FPL — consistent with current Medicaid law. Premiums would also be lowered for everyone else currently eligible for premium tax credits and a new cap on the total amount of income a person would have to pay would end the “subsidy cliff” under which a small change in income could result a large premium spike. This provision is particularly important of middle aged and middle-income adults who now face very high premiums as soon as their income crosses the 400% FPL threshold.
Conclusion
The Affordable Care Act has provided better access to health care and greater financial security to tens of millions of people. Yet premium affordability has remained a problem for many. For the first time in over ten years, Congress and the president have an opportunity to build on the foundation created by the ACA and they appear to be seizing it.
[i] Other steps include CTG, reduce OOP, expand eligibility to both ACA and Medicaid/ CHIP; continuous open enrollment at least for highly subsidized groups along with other steps to remove barriers and ease/ support enrollment