This is the last in a series of blogs discussing the policy priorities of the Center for Consumer Engagement in Health Innovation. Previous blogs have discussed health equity, population health, consumer protection, payment models and person-centered care models.
At the launch of our Center for Consumer Engagement in Health Innovation in January 2016, panelist Amy Berman, RN, Senior Program Officer at The John A. Hartford Foundation, described our current health care system as a “pre-Copernican” model, where all of the planets float around the health care system, and the patient is just one of them.
We need to re-align the health care universe, to place the consumer at the center.
To achieve this, we need to actively and meaningfully engage consumers in every aspect of health system transformation. The refrain “nothing about us, without us,” the cornerstone of the disability rights movement, should become the standard in health system redesign.
We were pleased to see that the Institute of Medicine’s report, Vital Signs: Core Metrics for Health and Health Care Progress identified “engaged people,” referring to both individual and community engagement, as one of four key quality domains. “Engaged people,” along with “healthy people,” “care quality” and “care cost” were recommended as the four domains in a “parsimonious” but comprehensive set of health metrics that could be adopted by public and private health programs and organizations.
At the Center, one of our key policy priorities is to advocate for structures for meaningful consumer engagement. We believe that this engagement must happen at three distinct levels – individual, system and policy. In practice, these translate to the need for engagement in the clinical setting, in health care organizations, and in federal and state policymaking.
The table below summarizes the goals of engagement at each of the levels and gives examples of specific policies that can help support these goals.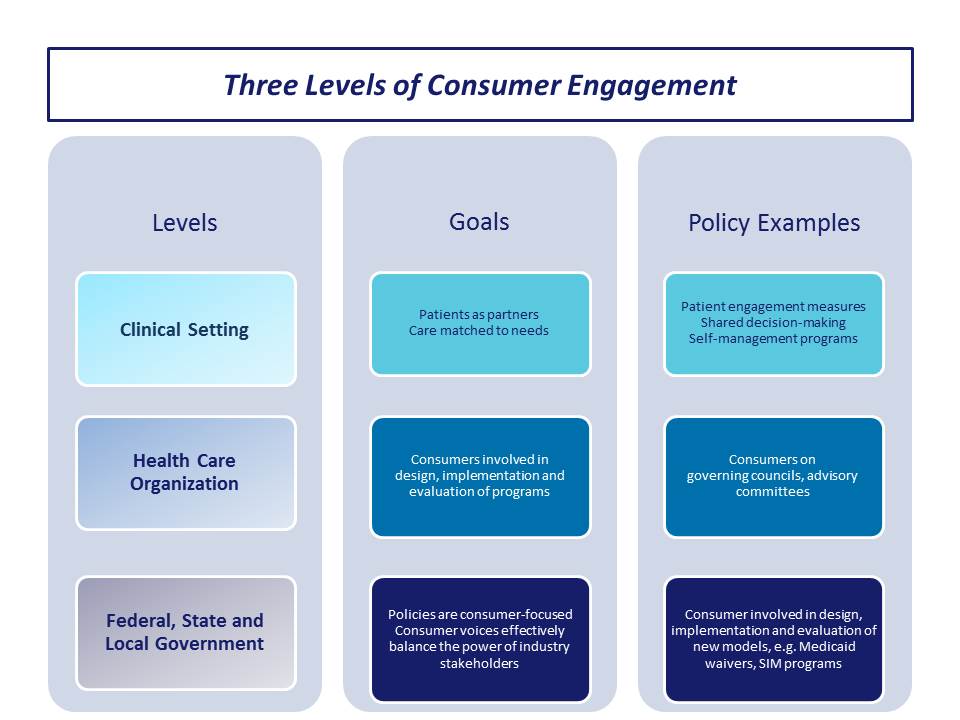
In the clinical setting, there are a number of tools available to help clinicians and patients work together in the pursuit of better patient engagement in their own care. For example, the Stanford Patient Education Resource Center has developed a Chronic Disease Self Efficacy Scale. There is also a proprietary Patient Activation Measure (PAM 13) and a two-question health confidence measure. We note that the Institute of Medicine’s Vital Signs report considered health literacy to be the best measure of patient engagement. We support the continued adoption of patient engagement activities, including shared decision-making and evidence-based self-management programs, in light of the body of evidence that shows that patients who are more engaged or activated have better health outcomes. There is also some evidence that shows an association with lower cost. We note examples of practices that have used patient engagement as a focal point for care redesign.
At the health care organization level, we support including consumers in governance of organizations and programs. For example, plans participating in Ohio’s dual eligible demonstration project (MyCare Ohio) are required to have a Consumer Advisory Council (CAC) in each region the plan serves. Community Catalyst has supported the work of Ohio Consumer Voice for Integrated Care (OCVIC), a statewide coalition of aging and disability advocates that organizes and educates MyCare Ohio beneficiaries. OCVIC has been heavily involved throughout the MyCare rollout in building a voice for MyCare beneficiaries and advocating for policy changes going forward.
We believe that strong consumer representation like this is critically important in the governance and quality improvement activities of health care organizations, including Accountable Care Organizations and health plans, and that this representation must be supported through training and appropriate levels of funding.
Finally, we believe that consumers must have a seat at policymaking tables. As Massachusetts was developing its dual eligible demonstration, it sought input from diverse consumer perspectives through focus groups and outreach sessions. This process was essential to shaping the design of the state’s care delivery model and demonstration proposal to CMS. At the urging of state disability advocates, Massachusetts established an Implementation Council which was charged with monitoring program access and quality, promoting transparency in program implementation, and assessing Americans with Disabilities Act (ADA) compliance. The council’s members were identified through an open nomination process. At least half of the slots are required to be filled by MassHealth beneficiaries with disabilities or their family members and the remaining slots were filled by representatives of hospital, provider, collective bargaining and advocacy organizations. The Implementation Council holds monthly meetings that are open to the public and has a workgroup structure to examine specific issues such as long-term services and supports.
In addition to formal structures, we advocate for inclusion of consumers at “ad hoc” gatherings and meetings. For example, I was pleased to be able to join a roundtable that Sylvia Burwell, Secretary of HHS, convened in Washington, D.C. in January 2016 to discuss consumer engagement.
The roundtable was a powerful and validating step toward recognizing the importance of steering our nation’s health care onto a more consumer-centered course. We hope to see more such moves at the federal, state and local levels.
At the Center we are dedicated to advancing consumer engagement at all three levels, and to putting the sun back where it belongs: in the center of our Copernican universe.
