With a year to go before Exchanges open for business, the pace of new guidance continues to pick up. Just this past week, HHS released guidance on State Partnership Exchanges. The Partnership Exchange is not an option presented in the Affordable Care Act (ACA), but rather a regulatory approach to giving states an opportunity to be included in Exchange development and management without establishing a State-Based Exchange (SBE). The Partnership model offers states a seat at the table in two areas: plan management and/or consumer assistance. In addition, a Partnership Exchange may serve as a stepping-stone to an SBE and allow some political cover for states that are slow starters on Exchange implementation.
Plan management involves many tasks related to the successful selection and administration of Exchange health plans. Specifically, the guidance details it as the development of qualified health plans (QHP) inclusive of certification, recertification, and decertification. As a reminder, QHPs must be certified by the U.S. Department of Health and Human Services (HHS) and face penalty of decertification if the plan does not comply with standards drafted by HHS and the state; plans must also be re-certified annually. In a Partnership Exchange, plan management also entails daily oversight and administration of QHPs.
States also have the option of managing the consumer assistance portion of the Exchange. This work includes day-to-day management of Navigators and the development and management of a separate Assister program. As a reminder, Navigators are guides that help people understand and enroll in the Exchanges. The Assister program is a not in statute but is a new optional program that is distinct from Navigators yet serves as an additional consumer assistance tool and can be funded through Federal Exchange grant dollars (you can find a handy chart about consumer assistance here). Finally, the state may also opt to be responsible for outreach and educational activities. With respect to consumer assistance in Partnership Exchanges, HHS will operate the call center and website and be responsible for funding and awarding Navigator grants in states.
The guidance sheds some light on the distinctions between what activities HHS will spearhead and what activities state governments will lead for the two options available in a partnership – plan management and/or consumer assistance. While a few questions remain, the guidance does present a helpful outline of activity responsibilities and a general timeline as we count down to open enrollment for Exchanges in October 2013.
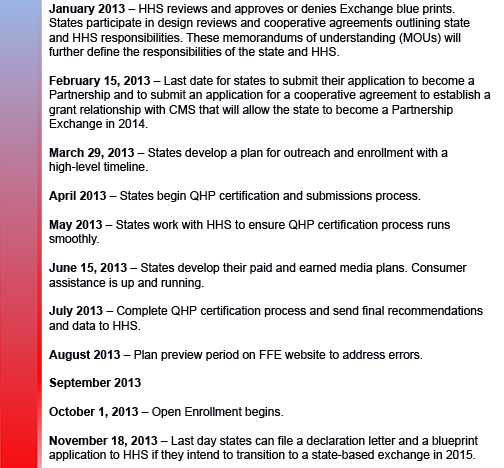
We thought that it would be helpful to highlight some of the necessary Partnership Exchange activities that will be underway in 2013. The dates presented in the guidance are not all deadlines but rather guideposts for states to follow in order to successfully launch plans and consumer support in time for open enrollment.
In addition, the guidance does outline in greater detail the approach for QHP certification for 2014 and is worth reviewing. Key highlights include the development of agreements between HHS and states, details about the amount of time that is allowed for HHS and state communications about certification, and data requirements for states. Tim Jost nicely summarizes them in his blog on the guidance, as does Christine Monahan on Georgetown’s CHIRblog. You can learn more about the state Partnership Exchange model and consumer strategies for a robust Exchange in a new paper by Community Catalyst, here.
With respect to consumer assistance, the guidance summarizes much of what we already know – however, the summary is helpful and better articulates the distinctions and overlap between Navigators and Assisters (referred to in the guidance as In-person Assistance). Some key highlights on consumer assistance from the include a description of responsibilities for development of training materials and how states may tailor the materials for their state; opportunities to fund Assisters through federal grant money (next application date is February 15); and a reminder all states will have a Navigator program that must be funded by the state. Please stay tuned for future discussion about the various tools available for consumer assistance.
Overall, the information in the guidance is a reminder states need to pick up the pace to meet the open enrollment deadline. That being said, HHS reminds us they will structure Exchanges where states do not.