Photo credit: Bigstockphoto.com
Much has been written about the terrible toll – current and projected – of the COVID-19 pandemic on the older adult population, and in particular, those living in nursing homes. Currently, there are roughly 1.3 million nursing facility residents, most of whom are older adults. This group is at very great risk for contracting the disease and is already paying a heavy price in the pandemic. The focus on this extremely vulnerable population is certainly warranted. In addition, more than three million older adults are living in close communal contact in independent living, assisted living and senior housing facilities.
Yet, another sub-population is also extremely vulnerable: the nearly seven million older adults living in the community [i.e., in their own home or apartment, rather than a larger institutional facility] who suffer from respiratory illnesses – asthma, Chronic Obstructive Pulmonary Disease (COPD), emphysema and other conditions.
A Highly Vulnerable Sub-Population
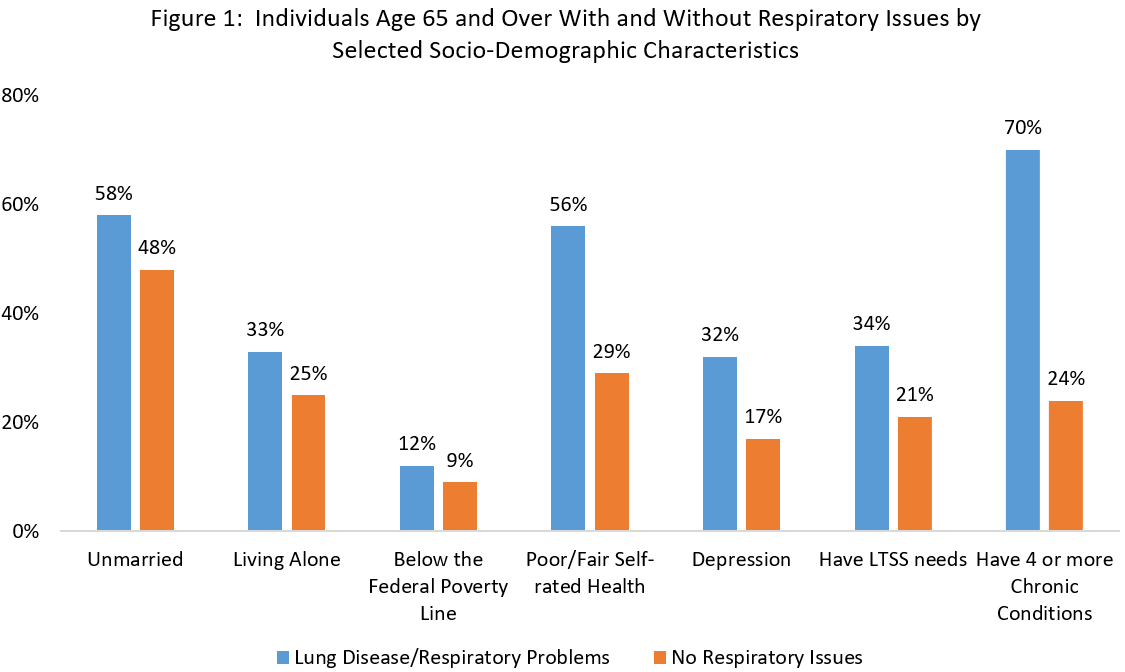
Part of what makes this population so vulnerable is that they have multiple additional risk factors in addition to their respiratory problems. Our analysis, which compares some of the key health and socio-demographic characteristics between groups with and without respiratory illnesses, shows that older adults living in non-institutional settings with respiratory illnesses are more likely to be unmarried, living alone and 1.3 times more likely to be living below the poverty line.
Not surprisingly, older adults with chronic respiratory issues living on their own in the community also suffer from additional health issues that place them at high risk. They are about twice as likely to report that their health is fair or poor, twice as likely to report depression, 1.6 times as likely to need long-term services and supports (LTSS) in their homes, and 2.9 times more likely to have four or more chronic conditions (inclusive of, and often medically related to, their respiratory conditions) than are those without respiratory issues.
Given the profile of these individuals, the current strategy for dealing with the virus – physical distancing – is unfortunately exacerbating other problems that already exist for many in this group, first among them, social isolation. There is a large body of literature documenting the negative health effects of social isolation. Thus, while physically distancing or isolating individuals is an absolutely essential measure to protect medically vulnerable older adults for a yet-to-be-determined span of time, over the long term it is virtually certain to aggravate other health issues for this population. During the current pandemic, non-urgent medical visits and chronic illness checkups are being significantly delayed or canceled. This means that even without contracting COVID-19, this population is facing increased health risks from reduced management of their existing respiratory disease.
What Can Be Done?
The coronavirus pandemic poses an elemental challenge to our society of how diligently we will respond to prioritize the safety and care of all groups who are at heightened risk, older adults being one such key group. We can meet this challenge in several ways:
- Testing: It is critically important that we prioritize older adults with known respiratory issues for coronavirus testing, wherever they live. Screening will save lives, as it will be possible to target resources to individuals who may be at the early stages of symptoms and illness onset, thus affording more potential for early intervention treatment options.
- Assessment: Providers should proactively assess older adults’ underlying medical and social conditions that pose a higher risk of death, should they contract COVID-19. This means proactively flagging all chronic conditions, particularly known respiratory issues, for all their patients’ providers in order to encourage proper vigilance and early treatment.
- Social Support: Supportive services providers must reach out to this population using telehealth approaches in order to combat isolation and loneliness. A schedule of “check-ins” with isolated older adults is vital to provide social connection and meaningful interactions, either by way of telephone calls or, if the person has access, through video technologies that facilitate face-to-face interactions (e.g., Zoom, Facetime, Facebook Messenger video chat, Skype, etc.).
- Basic Needs: Essential food and medicine must be delivered to these older adults in their homes so that they avoid potential exposure to the virus by going out, for the duration of time physical distancing needs to be practiced.
- Protection for Home Care Workers: Amid the national crisis of shortages of personal protective equipment (PPE), frontline workers providing LTSS to older adults in their homes lack essential protective equipment. These workers, and the people they dedicatedly care for, must be protected by prioritizing allocation of PPE to them. In addition, this workforce needs other protections: financial protections similar to those that were provided to 9/11 emergency responders; the ability to self-isolate and not come to work when sick; regular testing, and compensated respite days.
Even amidst the mounting reports of catastrophic transmission and fatality clusters within institutional settings, we must be proactive in monitoring and caring for the millions of older adults with pre-existing respiratory disease living on their own in the community. Let’s work on keeping them safe.
For more information, visit Family Caregiver Alliance www.caregiver.org, AARP.org and the Centers for Disease Control and Prevention (http://www.cdc.gov/).
Marc Cohen, Research Director at the Center for Consumer Engagement in Health Innovation, co-directs the LeadingAge LTSS Center@ UMass Boston. Jane Tavares is a Research Fellow at the LeadingAge LTSS Center @ UMass Boston.
