This post in our Health System Transformation series is an update of the Jan. 26, 2016 blog post titled, “How America’s Social Structures Affect Our Health.” This updated post adds some key policy prescriptions that are central to the vision of Community Catalyst’s new Center for Consumer Engagement in Health Innovation.
In the initial blog post of this series, we mapped out Community Catalyst's policy agenda for Health System Transformation (HST). In order to achieve our goals of better value for our dollars and better health for all, we believe it is necessary to think beyond the delivery of medical services. Often the factors that have the greatest impact on health don’t involve the health care system at all. For example:
- If you did not have a home or a refrigerator to store your insulin, how well would you be able to control your diabetes? Being provided with a safe place to store your medications would be the better solution, compared to waiting until you got so sick from high blood sugars that you needed to be hospitalized.
- If your child’s asthma is made worse by air pollution in your neighborhood or the dust in your home, wouldn’t addressing the living conditions — by the provision of a home air filter or by public health measures to improve regional air quality — be more effective than increasing the number of your child’s medications and trips to the emergency room?
- If a family doesn’t have enough to eat, wouldn’t food be the most important medicine?
Traditionally, the health care system has not taken on these and many other social and environmental factors that contribute to poor health, but we believe that must change. Social determinants of health — which encompass social, environmental and behavioral influences like access to healthy food and water, safe housing, employment/working conditions, gender and culture — play an important role in promoting health and potentially lowering health care costs, and must be addressed by health system transformation efforts.
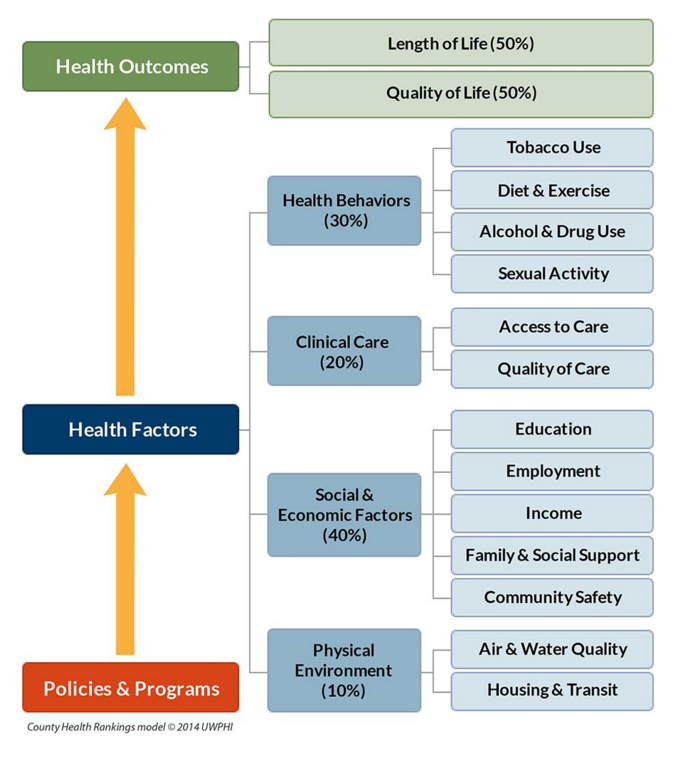
The County Health Rankings Model included in our report, The Path to a People-Centered System: Next Generation Consumer Health Advocacy, and reproduced below, nicely illustrates the many factors that contribute to health. Furthermore, a substantial body of research, including data compiled in The American Healthcare Paradox and “Leveraging the Social Determinants of Health: What Works?,” demonstrates that higher ratios of social-to-health care spending are associated with better health outcomes.
The U.S. health care system is the most costly in the world, but our population’s health outcomes are worse than those of most other Organization for Economic Cooperation and Development (OECD) countries. A driver behind this gap could be the relative “underspending” on social services compared to medical care: in the U.S., for every dollar spent on health care, only about $0.91 is spent on social services. In comparison, for every dollar spent on health care, OECD countries spend $2 on social services. Increasing spending on social services could help improve health, while decreasing health care costs. Across the country, there have been many examples of forward-looking programs that are working to direct resources to address social determinants of health:
- In Massachusetts, the Medical-Legal Partnership Boston, an interdisciplinary team of health care staff, attorneys and paralegals, provides direct legal assistance to low-income patients, ensuring their basic needs for housing and utilities are met. The impact of their services is significant: by connecting low-income families to utilities, food and housing services, they are able to demonstrate improved health outcomes for the population they serve.
- The Northwest Bronx Community and Clergy Coalition has a grant through the BUILD Health Challenge to work with Montefiore Hospital to address asthma in their community. The partners are working with tenant organizations in the Bronx to rehabilitate “sick” buildings to prevent and treat asthma that is linked to housing conditions.
- Maine Equal Justice Partners (MEJP), a legal aid organization, surveyed 1,000 low-income Maine residents to better understand their needs. The results showed that, by far, the greatest need was housing. Using this data, MEJP successfully advocated for increases in access to ongoing housing subsidies and is continuing to advocate, with the support of a newly-created Affordable Housing Working Group, to ensure greater access to affordable housing and therefore, a healthier population.
There are many more examples of initiatives that can improve the underlying health status of populations, but too often they lack adequate and stable funding. To address this problem, as health advocates, we need to broaden our partnerships to include organizations that work to secure affordable housing, promote access to healthy food, and address the other social and public health needs of a community. We also need to advance policies that can build support for addressing these issues right into the health care system, such as by:
- Ensuring that hospital community benefits programs (a requirement of non-profit hospitals in order to earn their tax-exempt status) help address the identified needs of their communities, including social supports and housing.
- Structuring new models of integrated health care delivery to include community-based organizations, who can then share in cost savings generated by achieving better health, as New Jersey has done with its Medicaid Accountable Care Organization model.
- Investing in organizations that assess patients’ needs and connect them to social support services in the community. One excellent example is Health Leads, which allows health care providers to prescribe basic resources like food and heat just as they do medications, then refers patients to advocates who help fill the prescriptions, working side-by-side with patients to connect them to the additional prescribed resources.
- Encouraging adequate payments for the housing, transportation, and social support services that people need to improve their health and ultimately reduce costs.
- Ensuring that payment models encourage prevention. One way to do this is to make sure that organizations delivering care are evaluated based on how well they are improving the health of the communities they serve, through the use of quality measures that assess community/population health. This can also be done by designing payment models like the all-payer model in Maryland that gives a fixed budget to hospitals, so that hospitals benefit if they keep people healthy.
- Directly supporting prevention and wellness activities. Massachusetts, as part of its 2012 comprehensive health care cost containment law, levied assessments on plans and providers to create a Prevention and Wellness Trust Fund to support population health interventions.
We have the most costly health care system in the world, but we don't get results commensurate with our level of spending. At the same time, relative to other countries we spend much less on addressing the social and environmental conditions that can lead to poor health. Addressing this imbalance must figure prominently in our Health System Transformation agenda if we are to be successful at improving the value we get for our health care dollars.
Note: Lauren Banks, was a contributing author to the earlier version of this blog post
